Patient population
Clinical characteristics are presented in Table 1.
Between November 2017 and November 2018, 1140 patients underwent spinal surgery in our department due to various pathologies. Of them, 526 patients (292 males, 234 females) were included in this study analysing complications. The patient’s median age was 67 years (range: 13–96).
General characteristics of the patient population indicated it to be overweight with a mean BMI (Body Mass Index) of 27 (range: 12–52). The mean ASA score was 2, reflecting a moderate but definite systemic disturbance. Mean DC (Diagnosis Count) was 2 and range 0–12, leading to a mean CCI of 2 (range: 0–17) highlighting the likelihood of mortality within a 10-year period in 48% cases.
Of the subjects, 16% were smokers and 15% admitted to alcohol abuse (on a daily basis). Regarding co-medications, 30% were under anticoagulant medication, which was continued perioperatively in 9%.
The main diagnoses were degenerative (50%), tumour (22%), traumatic fractures (13%), infections (10%), and others (5%).
Surgical procedures
Emergency surgeries (within 24 h) were performed in 12% of the patients with a mean duration of 142 min (range: 11–440). Operations comprised 3 vertebral segments on average and were instrumentations in 59% (13% percutaneous vs. 87% open instrumentation). Regarding the location of the surgeries, 60% were performed on the lumbar spine, 26% on the cervical, and 26% on the thoracic spine.
The mean blood loss was 638 ml (range: 0–8000 ml). Thereby, the main diagnosis tumour correlated with higher blood loss (mean: 1149 ml within this subgroup).
Complications and risk factors
Within our study collective, intraoperative complications emerged in 26 cases (4.9%). These included accidental Dural lesions (19 patients), injury of the vertebral artery (3 patients), premature termination of surgery due to unexpectedly high blood loss or cardiopulmonary instability (2 patients), accidental rhizotomy (1 patient), and cement leakage (1 patient).
Postoperatively, 135 (25.7%) patients suffered complications within 30 days. Of those, 83 were surgical complications and 52 were systemic. Interestingly, 19% of these patients had already been discharged when the complications occurred (median time of discharge to complication: 0.5 days [IQR 0–8.5 days]). The complications are recorded in Table 2. Risk factor analysis is presented in Table 3.
Furthermore, 61 patients (12%) required revision surgery within 30 postoperative days (median time to revision surgery: 11 days [IQR 5–15 days]).
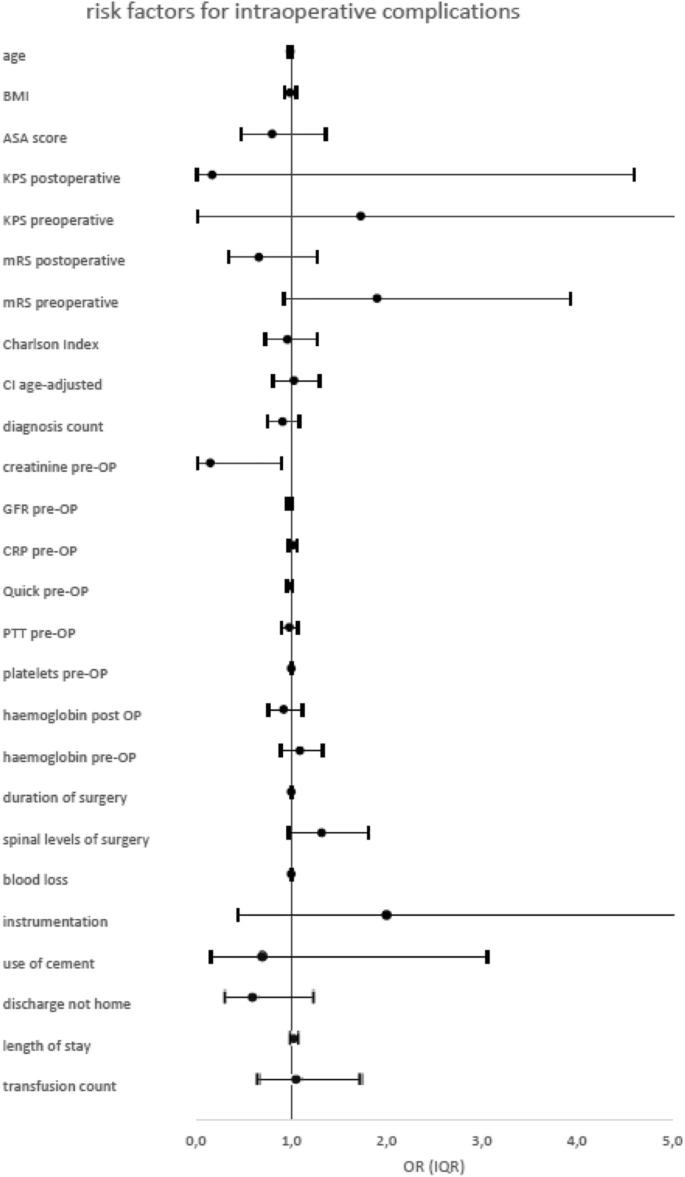
Intraoperative complications
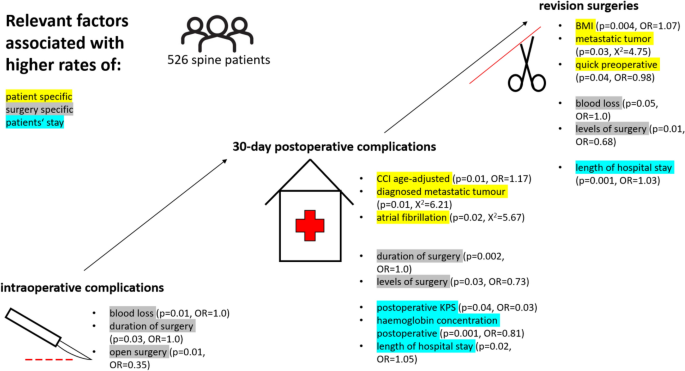
The multivariate logistic regression analysis revealed blood loss (p = 0.01, OR = 1.0) and duration of surgery (p = 0.03, OR = 1.0) as independent risk factors for intraoperative complications.
The spinal instrumentation (p = 0.37), previous spine surgeries (p = 0.45), or other patient-specific risk factors did not influence the rate of intraoperative complications.
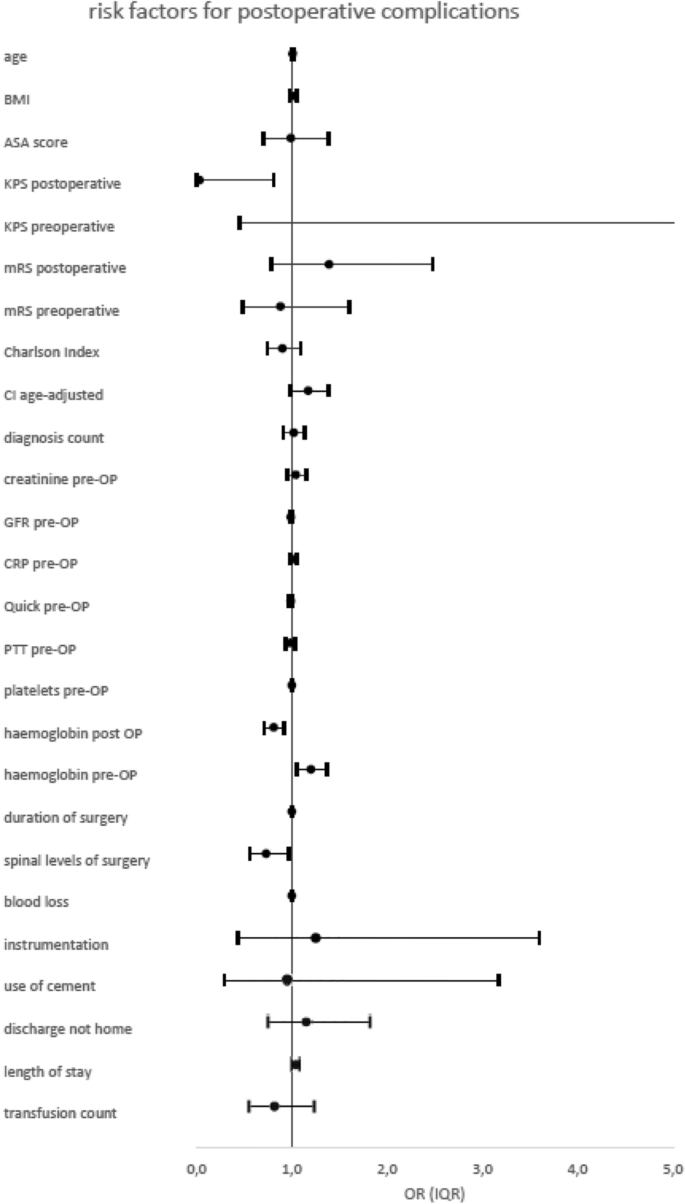
Postoperative complications
Concerning postoperative complications, the following patient-specific risk factors could be identified: postoperative KPS (p = 0.04, OR = 0.03) and CCI age-adjusted (p = 0.01, OR = 1.17). Patient age showed borderline significance (p = 0.069, OR = 1.01).
The relevant blood parameters were haemoglobin concentration postoperative (p = 0.001, OR = 0.81) and haemoglobin preoperative (p = 0.01, OR = 1.20).
Analysis of surgery itself revealed that spinal levels of surgery (p = 0.03, OR = 0.73) and the duration of surgery are strongly correlated with postoperative complications (p = 0.001, OR = 1.0).
Furthermore, the duration of hospital stay (p = 0.02, OR = 1.05) was strongly associated with higher complication rates. The median length of hospital stay was double in the case of complications: 15 days (IQR 6–23) with complications; 7 days (IQR 3–12) without complications. Complication rates according to discharge destination and frequency were: home (21% complications), another department at the same hospital (20% complications), another hospital (38% complications), rehabilitation centre (35% complications) and death during follow up (100% complications).
Surgeries combining cervical and thoracic spine or thoracic and lumbar spine treatments showed significantly more postoperative complications than interventions on the cervical, thoracic, or lumbar alone. The use of navigation devices showed no significant influence on postoperative complications.
Patients diagnosed with metastatic tumour (p = 0.01, χ2 = 6.21) or atrial fibrillation (p = 0.02, χ2 = 5.67) developed significantly more postoperative complications.
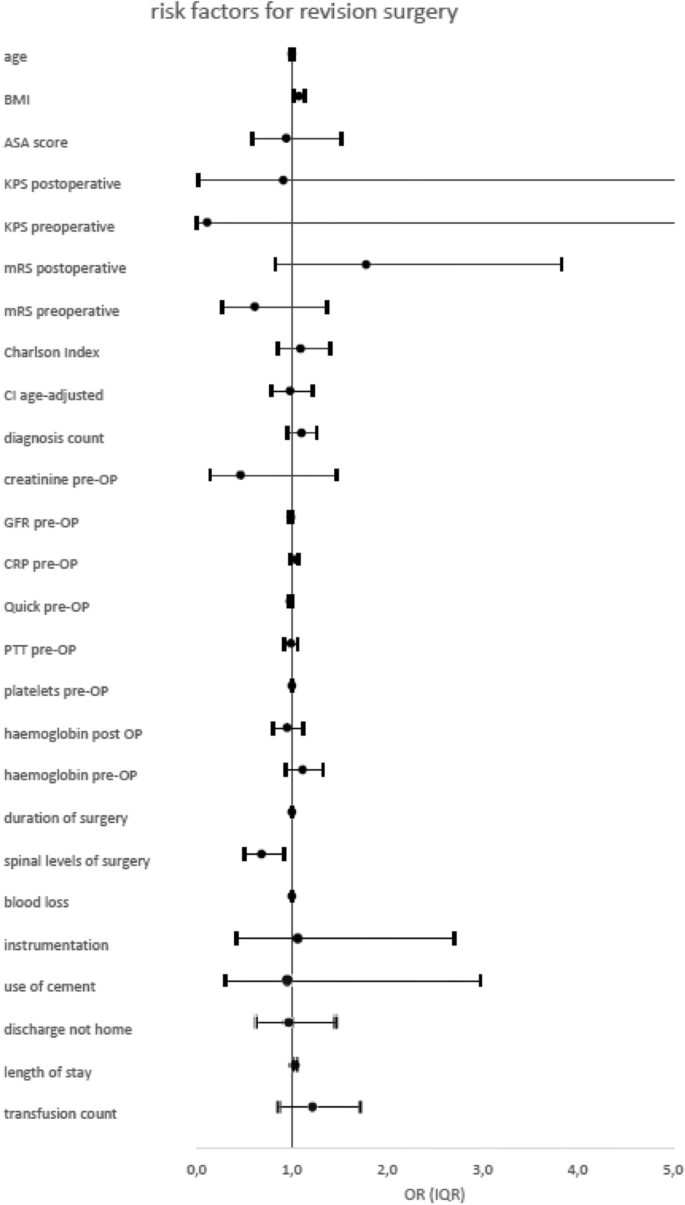
Revision surgeries
Concerning revision surgeries, patients with higher BMI underwent revision surgeries more often (p = 0.004, OR = 1.07). Other patient-specific risk factors were not predictive for revision surgeries.
Confirming the results of postoperative complications, the more spinal levels were operated on (spinal levels of surgery p = 0.01, OR = 0.68) and the more blood loss occurred (blood loss p = 0.05, OR = 1.0) the more revision surgeries had to be performed.
Length of hospital stays also correlated with the number of revision surgeries (p = 0.001, OR = 1.03).
Patients with metastatic tumours also were revised more often (p = 0.03, χ2 = 4.75).
Figure 2 provides an overview of the significant parameters.
We graded the complications in this study into “major”—requiring revision surgery or leading to transferal to intensive care unit and “mild” for complications that could be resolved completely within days after surgery.
Interestingly, there is no significant difference regarding age within the groups. Mean age in the group with mild complications was 68 years, in the group of major complications it was 65 years, respectively. According to the previous presented results, analysis showed that the group of major complications showed higher BMI values than did the mild complication group (mean 29.1 versus 25.6).